LIFESTYLE ADVICE TO SUFFERERS
They should take measures to prevent any other liver complaints.
Vaccination against Hepatitis A & B is advisable - There is now a combined vaccine
Use caution with alcohol - the recommended level is a maximum of 4 - 5 standard drinks a week.
Avoid raw oysters.
Beware of fad diets e.g. liver cleansing diet, etc.
Take care with Vitamin C, which turns iron into a more toxic form. There have been deaths recorded with high levels of vitamin C taken regularly. If you decide to take any vitamin C then you should take vitamin E as well.
OSTEOPOROSIS
Bone thinning is more common with liver disease, particularly haemachromatosis. Good advice includes walking (weight bearing exercise), diet to include calcium rich foods or a calcium supplement. There are already drugs on the market that are counter-acting osteoporosis and actually lead to bone thickening - phosphanates - It is usual to go on a course for about 2 weeks, then a couple of months off.
ARTHRITIS & HAEMACHROMATOSIS
There are three kinds of arthritis which may be associated with haemochromatosis:
DEGENERATIVE (wear & tear)
In degenerative joint disease there is uniform narrowing of the space between the joints, bony spurs develop and cavities form over time, the iron in the joints oxidises - we literally get rusty joints. This activates enzymes, which eat up the cartilage, which provides smooth surfaces for joint to rub against joint.
CHRONDOCALCINOSIS (where calcium is deposited in the joints)
Chrondocalcinosis is a build up of calcium and affects most joints. The iron inhibits the enzymes which make calcium soluble.
INFLAMMATORY joint disease consists of occasional or persistant swelling of the soft tissues. In this type, lymphocytes migrate to joints, iron stimulates blood cells to attack the joint structure, and once it is in the joint, it cannot exit.
BALTI CURRIES AND IRON
The use of cast iron cookware has been shown to increase the iron content of food, and the bioavailability of this contaminant iron is shown to be high. Although the use of cast iron cookware is not particularly high, it seems to be gaining in popularity.
It is specifically used in the preparation of an Indian cuisine known as BALTI, where food (a curry) is served straight from a small cast iron wok.
A study was made to compare the iron content of these meals prepared in a cast iron balti wok with food as bought.
| Food iron as purchased | Iron after cooking | |
|---|---|---|
| Vegetable Curry | 0.86 (mg/100g) | 10.67 (mg/100g) |
| Chicken Balti | 1.54 (mg/100g) | 12.73 (mg/100g) |
| Vegetable Balti | 1.46 (mg/100g) | 6.15 (mg/100g) |
COMMENT
These data suggest that the iron intake of people consuming traditional balti meals could be extremely high, falling well outside the normal range of dietary intake (10-12 mg/day). For example, a meal of chicken and vegetable balti dishes could provide about 50 mg of iron. Giving dietary advice on iron is not easy as the absorption of iron from meals varies greatly.
One of the richest sources of well absorbed iron is liver (7 mg iron/portion), but this contains considerably less iron than meals cooked in the balti wok.
People with haemochromatosis should be advised to avoid balti curries prepared in cast iron cookware.
This information was provided by a Birmingham Co.(UK) firm which supplies balti curries.
by Jeanette Dixon
Coping with the chronic conditions that may accompany haemochromatosis can seem quite daunting at times. Diabetes, (sometimes referred to as 'bronze diabetes'), develops in about 65% of people with haemochromatosis.
It can occur as a result of damage to the pancreas as well as a genetic predisposition. It is more likely to develop in those who already have a family history of diabetes.
Removal of excess iron stores can sometimes improve mild non-insulin dependent diabetes, but people who need insulin usually need to continue with this treatment. Tablets or insulin may be needed to keep blood sugars at acceptable levels. But diet and exercise are still important cornerstones of effective diabetes management. The diet for diabetes is one that all Australians should be eating. This includes foods that are low in fat, high in fibre and low in sugar. With haemochromatosis, it is also wise to avoid iron-rich foods.
Complications arising from diabetes can include eye damage, heart disease, nerve and circulation problems in the feet and legs, kydney damage and impotence. Learning to balance food, exercise and medication to keep blood sugar at acceptable levels will help to prevent or delay complications. Your Doctor, Diabetes Nurse and Dietician can all help with fine-tuning these aspects. Aim to keep your blood sugar levels between 3.5 and 8.0 mm/L. Use a modern blood glucose meter to check your levels regularly. These simple, compact and precise instruments will provide valuable feedback and help keep you on track.
If all this gets a bit overwhelming at times, take heart! The rewards of having your diabetes under good control, more than pay for the extra effort expended. Forming good partnerships with appropriate health professionals will give you the confidence to put yourself in the 'driver's seat' and reap the benefits of improved health.
Jeanette Dixon is a registered nurse with a background in
diabetes education. She works as a research assistant in the Queensland Institute
of Medical Research.
The treatment of Genetic Haemochromatosis (GH) consists of lifelong phlebotomy or venesection therapy. Venesection is weekly at first to remove the excess iron, and this is followed by a maintenance programme with less frequent venesection to prevent re-accumulation of iron in affected organs.
DIETARY IRON
As the genetic expression leading to iron overload is so strong, an iron-reduced special diet is of little benefit in the prevention of reaccumulation of iron in the maintenance phase.
A low iron or iron restricted diet cannot replace the maintenance phlebotomy program.
This sort of diet could also lead to deficiencies in other important nutrients. However it is recommended that you minimize the intake of foods which are especially high in iron, or which are fortified with iron, and any supplements or tonics containing iron.
FOODS HIGH IN IRON
The highest sources of dietary iron are:
The offal meats - liver, heart and kidney: and foods prepared from these such as pate, liverwurst & haggis.
Black pudding - which is made from pigs blood
Oysters and mussels
FOODS FORTIFIED WITH IRON
Many breakfast cereal are fortified with iron, so read the ingredients list on the pack. Iron may be listed as MINERAL (IRON) or as an iron salt eg. FERROUS PYROPHOSPHATE.
Some chocolate powder drinks are also fortified, along with sports drinks, and baby cereals and formulae.
Some non-fortified alternatives to the above are:- porridge or mini-wheats, Quik, and cordials.
It is recommended that you do not consume either high dietary iron foods or iron fortified foods as part of your regular diet.
SUPPLEMENTS AND TONICS
Some supplements and tonics contain iron and/or vitamin C.
Check the ingredient list before using any supplement or tonic.
Supplemental multivitamins containing vitamin C are not recommended as: vitamin C enhances the absorption of iron, and large amounts of this vitamin can increase the damage iron can do to the heart.
NOTE: there is no need to restrict food sources of vitamin C, i.e. fresh fruits and vegetables, as these do not contain excessively large amounts of vitamin C.
ALCOHOL
As the liver is the organ first affected in Haemochromatosis, alcohol is not recommended as it can increase liver damage.
INHIBITORS OF IRON ABSORPTION
Some compounds found naturally in foods inhibit the absorption of iron. The phytates in wholemeal cereals and the tannins in tea are known to inhibit iron absorption. However, it is not recommended that you drink unusually large amounts of tea with meals, as this may affect the absorption of other minerals.
If you have diabetes, or any condition requiring specific dietary advice, please consult a dietitian.
HEALTHY EATING
It is especially important that individuals with haemochromatosis have a nutritious, balanced diet which provides all the essential nutrients needed to promote health and well-being. Do not unnecessarily restrict the intake of any foods or groups of foods from your diet, as this may lead to deficiencies in some nutrients. This is particularly important, as you will lose some nutrients other than iron with repeat phlebotomy, and these must be replaced with the foods you eat.
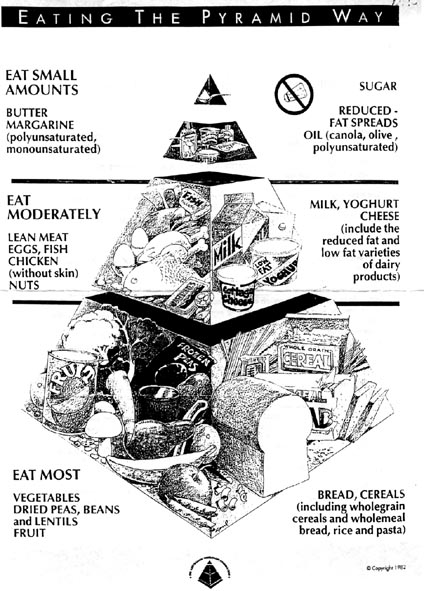
Eating a variety of foods in the proportions shown in the Australian Nutrition Foundation's HEALTHY EATING PYRAMID is the safest way to do this. Eating the Pyramid way will ensure that you are obtaining in the correct proportions, all the nutrients that your body needs to function.
A lifestyle which combines eating the Pyramid way, with regular moderate exercise such as walking or swimming is the best way to promote health and well-being. This will also help to maintain a healthy weight. Discuss any exercise program with your doctor before commencing.
EATING THE PYRAMID WAY
The healthy eating pyramid, as shown below, is divided into 3 sections to help you choose foods in the right proportions to promote health and well-being. The three sections are as follows:-
THE "EAT MOST FOODS"
These foods are at the bottom of the Pyramid and should make up the major part of each meal. Include these foods in all your meals, and use them as between meal snacks.
*Breads and cereals, including wholemeal bread and wholegrain cereals, rice, barley and pasta.
*Vegetables - fresh, canned or frozen. Dried peas, beans and lentils.
*Fruits - fresh, canned, frozen or dried.
These foods are low in fat and high in dietary fibre. Breads and cereals are the most important source of vitamin B1 in the diet, and they provide starch, protein and other B group vitamins such as vitamin B6, folate and riboflavin.
Vegetable and fruit provide almost all the vitamin C in the diet. The yellow and orange vegetable and fruits are important for the body's supply of vitamn A, and the green leafy vegetables supply folate.
It is impoprtant to include a wide variety of fruits and vegetables in the diet and not exclude any group such as spinach which contains iron. (the iron in vegetables is not as efficiently absorbed as that in red meat.
"THE "EAT MODERATELY" FOODS
*Milk, yoghurt and cheese, including reduced fat and low fat varieties.
*Lean meat, chicken (without skin), fish, eggs, nuts.
Both groups of foods are important sources of protein, but they also contain fat so it is a good idea to choose varieties with less fat, and prepare foods such as meat, chicken and fish without fat, or with only small amounts of fat.
The dairy foods provide most of the calcium in the Australian diet. They also provide B group vitamins, particularly riboflavin (vitamin B2)
Meat, chicken and fish are good sources of iron, with red meat having the highest Iron content. They are also the best sources of the mineral zinc and a good source of the B group vitamins, especially B12.Have 1 serve of the meat group a day to ensure adequate intake of all important nutrients. Select from either meat or chicken or fish or eggs. (1 serve = 100g of meat or 2 eggs)
FOODS TO EAT IN SMALL AMOUNTS
*Butter, polyunsaturated and monounsaturated margarines and reduced fat spreads.
*Oils (olive, canola and polyunsaturated)
*Sugar and foods with added sugar, eg. cakes, chocolate, soft drinks.
*Avoid the addition of salt in cooking and at the table.

This page is still under construction, and a glossary of terms is planned, as well as more articles. Keep checking!
You can e-mail the author on honsec@lycosmail.com
Last Updated 7July 1999